B.E. Smith Team | April 10, 2018
Healthcare Leaders Tackle the Future and Change at ACHE Congress
The American College of Healthcare Executives (ACHE) Congress annually probes a broad range of issues facing healthcare leadership. This year’s conference did not disappoint, providing extensive coverage of management, clinical, and technology topics. B.E. Smith was in attendance, and this Executive Brief highlights five particularly noteworthy themes and topics.
Seek Sustainable Change
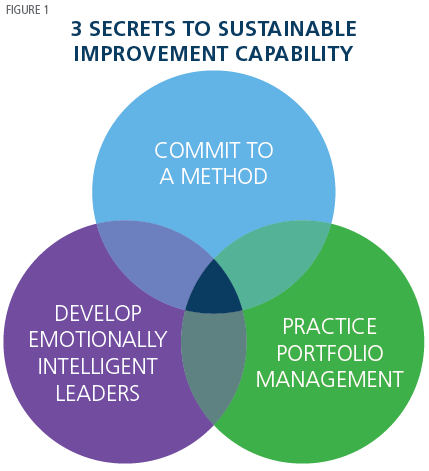 Managing change as the industry undergoes transformation is always a primary focus at ACHE. Several presenters homed in on the need to create sustained change to be effective. In “Three Essential Elements for Sustained Improvement,” Ian Lazarus, President and Chief Executive Officer of Creato Performance Solutions, described strategies to drive lasting change. (See Figure 1.)
Managing change as the industry undergoes transformation is always a primary focus at ACHE. Several presenters homed in on the need to create sustained change to be effective. In “Three Essential Elements for Sustained Improvement,” Ian Lazarus, President and Chief Executive Officer of Creato Performance Solutions, described strategies to drive lasting change. (See Figure 1.)
First, commit to formal improvement methods such as Lean and Six Sigma. Commitment means more than generating a plan. It also requires allocating sufficient resources, dedicating appropriate staff, and aligning incentives. Second, develop leaders who possess “emotional intelligence” given that “organizational change is an emotional event” and broad acceptance is needed to sustain improvements. Finally, “do the right things as well as do things right.” Concentration on quick wins or projects with minimal impact “erodes credibility.” Lazarus urges project portfolio management as a toolset to guide the right choices.
The session “Once is Not Enough: How to Sustain Cost Savings to Thrive,” focused on the important topic of sustaining change. Bonnie Levin, Assistant Vice President Pharmacy Services, Raymond Lake, Director of Pharmacy Operations at MedStar Health, along with Kathy Chase, Director of Drug Cost Control at Cardinal Health, applied the concept to the critical area of cost control.
Long-run financial benefits accrue only to those leaders who embed a “culture of continuous savings” throughout their organizations. Describing a “multimodal” strategy, the session offered three strategies to ensure cost savings measures stick.
- Working on multiple fronts
- Standardizing and centralizing savings across the enterprise
- Maintaining continuity – “never accept that you are done”
Build a High-Reliability Culture of Safety
One crucial area where hospitals have sought sustained improvement is in patient safety. As expected, this topic had extensive visibility at ACHE. The need to create a “high reliability organization” surrounded by a deep “culture of safety” was a consistent message throughout the Congress. ACHE has supported this effort through its report “Leading a Culture of Safety: A Blueprint for Success.”
Dr. Peter Pronovost, Senior Vice President at Johns Hopkins Medicine and Director of Armstrong Institute for Patient Safety and Quality at Johns Hopkins, set the stage in his keynote “Patient Safety is Everyone’s Job.” Defining a high reliability organization (HRO) as one that “pursues excellent performance under complex and dynamic conditions,” Dr. Pronovost identified four narratives that hinder its attainment:
 Harm is inevitable rather than preventable
Harm is inevitable rather than preventable- Safety is a local project rather than an integrated operating management system
- Safety and productivity are based on the heroism of clinicians rather than design of systems
- Total cost of care is not my responsibility
A “new mindset” must take hold in which safety is the responsibility of everyone from the board to the patient. Leadership’s role is to “use all levers” to link people and provide the clarity, feedback, and resources needed for maximum reliability.
Joanne Sorenson, Chief Nursing Officer and Vice President of Patient Care Services at UPMC Northwest, and Anne Pedersen, Director of Nursing at UPMC Harmot, picked up the theme in “From Macro to Micro: Using Shared Governance as a Vehicle to Create a Safety Culture.” The two extended Dr. Pronovost’s HRO definition to encompass five characteristics. (See Figure 2.)
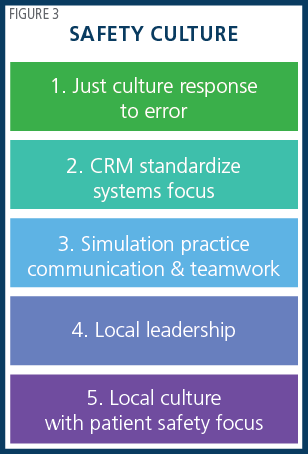
“Shared governance” is required, with an empowered staff “formally organized to make decisions about clinical practice standards and quality improvement.” Driving safety throughout the organization is key, and there is an “emerging recognition that a safety culture is local and micro.” The presenters offered five strategic components of a safety culture as shown in Figure 3.
 The session “High-Reliability Organizations: Preparing for Success in Uncertain Times” focused on high reliability as the “chassis” for safety. The session was led by Joel Bundy, Vice President of Medical Affairs at Sentara Leigh Hospital, and Craig Clapper and Gary Yates, both partners at Press Ganey. According to the speakers, the essence of building a sustained culture is ensuring that all practices are “performed as intended consistently over time.” They urged “evidence-based leadership” with five priorities:
The session “High-Reliability Organizations: Preparing for Success in Uncertain Times” focused on high reliability as the “chassis” for safety. The session was led by Joel Bundy, Vice President of Medical Affairs at Sentara Leigh Hospital, and Craig Clapper and Gary Yates, both partners at Press Ganey. According to the speakers, the essence of building a sustained culture is ensuring that all practices are “performed as intended consistently over time.” They urged “evidence-based leadership” with five priorities:
- Message on reliable safety and quality
- Support operations
- Build engagement and accountability
- Create and maintain reliable systems
- Learn as a team
Physician Alignment a Critical Success Factor
Physician alignment with organizational strategy is an essential and central tenet of value-based care. A coordinated care delivery model with engaged clinicians is the ideal. It has been a challenge for many organizations to achieve, and several sessions probed this vital issue.
In “Getting Physicians More Involved: One Hospital’s Story,” Carson Dye, President and Chief Executive Officer at Exceptional Leadership LLC, and David Zechman, President and Chief Executive Officer at McLaren Northern Michigan Hospital, looked at ways to gain involvement in clinical integration efforts and identify change champions. Barriers include relatively low physician engagement levels, growing feelings of burnout, and a general sense that “they are excluded from healthcare’s value efforts.” Leaders should focus on involvement, which is far deeper than simply soliciting physician input.
The speakers asserted that “uncoordinated, piecemeal efforts are insufficient.” Resist token leadership roles and overemphasis on financial incentives. Physicians ultimately want “emotional attachment” to a shared vision and an organizational “agenda they will embrace.” McLaren Hospital used a Physician Leadership Academy to promote comprehensive involvement. A curriculum initially designed to develop leaders quickly gave way to one offering involvement in “meaningful projects to enhance team skills and provide real-world leadership experience.”
Which physician leadership competencies should be developed? Britt Berrett, Director of the Center for Healthcare Leadership at the Jindal School of Management, answered this question in the session “Physicians Come Third: Leading Change with Physicians.” Berrett observed that “many new physician leaders struggle as Vice Presidents of Medical Affairs, Chief Medical Officers, and other senior positions,” despite superior academic achievement, training, and even gaining advanced management degrees. Berrett suggested that physician leaders need four crucial skills to become effective change agents. (See Figure 4.)

Finally, in the session “Proven Strategies for Tackling Low Physician HCAHPS Scores,” First Physician Corporation’s Lissa Singer, Chief Quality Officer, and Brian Tsang, President and Medical Director, joined consultant Bo Snyder in discussing the importance of satisfaction scores. The session’s focus was primarily on the impact and influence doctor-patient interactions have on satisfaction scores. HCAHPS and other satisfaction measures increasingly determine reimbursement, so intense leadership focus on helping physicians is critical. However, the session cautioned leaders not to nag doctors about low scores, fail to hold non-medical staff accountable, or begin campaigns without crucial buy-in. Instead, the presenters offered four best practices:
- Create expectations for high performance
- Provide information on what and how to change
- Make the right tools available
- Prompt doctors to begin the journey by asking, “How do you know you are doing a good job?”
Leadership Development for a Rapidly Changing Future
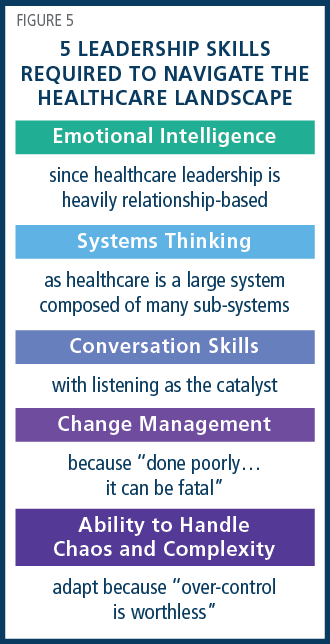 Putting the right leadership in place has never been more urgent as the pace of industry transformation accelerates. Meeting tomorrow’s needs was a topic of considerable interest. In “Leadership Competencies for an Unknowable Future,” George Washington University’s Dr. Leonard Friedman, Professor and MHA Program Director, and Wayne Psek, Assistant Professor of the Department of Health Policy and Management, discussed the uncertainty created by major “tectonic” shifts in the healthcare landscape. The two speakers identified five leadership skills required to navigate the terrain. (See Figure 5.)
Putting the right leadership in place has never been more urgent as the pace of industry transformation accelerates. Meeting tomorrow’s needs was a topic of considerable interest. In “Leadership Competencies for an Unknowable Future,” George Washington University’s Dr. Leonard Friedman, Professor and MHA Program Director, and Wayne Psek, Assistant Professor of the Department of Health Policy and Management, discussed the uncertainty created by major “tectonic” shifts in the healthcare landscape. The two speakers identified five leadership skills required to navigate the terrain. (See Figure 5.)
Future requirements were also spotlighted in “Preparing Healthcare Leaders for the Decade to Come,” by Andrew Garman, Chief Executive Officer at the National Center for Healthcare Leadership and Associate Chair at Rush University, Joseph Cabral, Chief Human Resources Officer at Partners HealthCare, and Joseph Moscola, Senior Vice President at North Shore-LIJ Health System. Examining several healthcare trends, the speakers proposed four as most impactful:
- Enhancing capacity for adaptive change
- Social determinants of health as emerging service lines
- Consumers as partners
- Broadening engagement
Preparing leaders to capitalize on these opportunities demands “evidence-based strategies” developed from “advanced workforce analytics” to build strength in transformation, execution, relationships, and boundary spanning.
The always provocative Jonathan Bush, President and Chief Executive Officer of athenahealth, challenged leaders in the session, “The Cost of Being Average: Lessons for Next-Generation Healthcare Leaders.” Bush urged healthcare executives to avoid “upper right quadrant syndrome” in which organizations “protect and defend” their markets and positioning rather than “compete and innovate” to counter growing competition from care in non-traditional settings. Bush offered three chief recommendations:
- become virtualized
- free up capacity by eliminating non-core competencies
- generate new business to grow share
Artificial Intelligence Offers Great Promise
Healthcare is becoming digital as technology advances at a staggering rate. Artificial Intelligence (AI) is one area making major strides. In “Changing Healthcare through the Power of Cognitive Computing,” Byron Scott and Tina Moen, both Deputy Chief Health Officers at IBM Watson Health, explained how AI encompasses several technologies such as machine learning and natural language processing to analyze massive data sets from diverse sources. The payoff is conversion of previously “invisible” data and knowledge into actionable insights. What the speakers term “cognitive computing” becomes “supportive of the human side of the equation.” This human-machine combination is creating “augmented intelligence” leveraging what each does best. (See Figure 6.)

Organizations need a plan and vision for analytics. That message was conveyed in “Successfully Deploying Analytics with Big Data and Artificial Intelligence Using Mobile Apps.” Vijay Venkatesan, Chief Data Officer for Providence St. Joseph, advised leaders to focus on three core elements of a data plan:
- Interlinked data inputs – mine clinical and administrative information
- Analytic models – outcomes analysis, disease management
- Decision support tools – treatment guidelines, drug interactions and more Venkatesan believes ROI is optimized in an “opportunity zone” comprised of “new responses to old questions” and “new insights to new questions.” (See Figure 7.)

Conclusion
Sustaining change, creating a safety culture, engaging physicians, ensuring future-oriented leadership development and reaping the benefits of AI – these five themes reflect the valuable breadth and depth of insights offered at this year’s ACHE Congress. The strategies provided in the sessions and highlighted in this executive brief provide healthcare executives a path to drive success in their organizations.
Read More