B.E. Smith Team | October 17, 2017
2018 Environmental Scan
Finding common themes and insightful trends in the health care field in this time of transformation and uncertainty can be challenging. But we must if we want to be proactive and shape events rather than merely react to them. Understanding the current climate and the direction of health in America will help us in our work to shape the health care delivery system of the future.
The legislative and policy work happening in Washington, D.C., and 50 state capitals is not the only driver of environmental changes. Advances in science, technology and information management; new models of care; changes in consumer preferences; and the growth of chronic conditions also play a large role. Addressing these issues provides us with the opportunity to find the best solutions for our patients and communities.
The American Hospital Association and America’s hospitals and health systems are seizing this moment and working to ensure:
- Coverage and access for all.
- High-value care.
- Patients, families and other stakeholders are involved as partners.
- Well-being and prevention.
- Services that are provided in a coordinated, seamless manner.
We have organized the trends that will be felt in 2018 and beyond through the lens of this vision: ACCESS, VALUE, PARTNERS, WELL-BEING, COORDINATION. These five commitments are the basis of the AHA strategic plan and touch all hospitals and health systems, even while each hospital’s path to achieving these ideals may differ. We hope that hospitals and health systems use this Environmental Scan to address the trends in health care and to tailor strategies to specific community needs.
While we work to advance health in America through our commitments, we cannot ignore the political climate in which health care has become a key focal point. Our advocacy strategies include grassroots efforts to spread our message through mobilization of millions of individual supporters, grass-tops action to amplify our voice through key media and stakeholders, sustained engagement with top policymakers by our advocacy team, data-driven research regarding the impact of potential policy changes, and focused advertising through a variety of media.
We work hand in hand with our members, state, metropolitan and regional hospital associations, national health care organizations and other stakeholders to develop and implement our strategy. We have developed a forward-thinking advocacy agenda that aims to positively influence the environment for patients, communities and the health care field.
Our field knows how to be nimble, stay focused and manage change. These traits will help us to navigate the road ahead. We have the opportunity to shape our future to fulfill our vision of a society of healthy communities where all individuals reach their highest potential for health. Thank you for your efforts to achieve this vision.
Rick Pollack
President and CEO
American Hospital Association
AFFORDABILITY
“Many of the efforts to restructure our health care system stem from the idea that health care should be affordable to all Americans. We at the AHA have to ensure that proposed reforms provide real solutions to the problem. We must do our part to provide high-quality health care in an efficient way and promote value-based models of care that reduce costs.”
JAMES H. SKOGSBERGH
President and CEO
Advocate Health Care
2017 Immediate Past Chair
EQUITY OF CARE
"Together as a field, it’s vitally important that we understand the different cultures, customs and languages that are unique to our communities in order to help with the physical, emotional and spiritual dimensions of healing. The AHA’s Equity of Care campaign seeks to strengthen the commitment of hospitals and health systems to eliminate health and health care disparities that continue to exist for our patients. Through these efforts, we’re working hard to ensure that every person in every community has the opportunity to reach their highest potential for health.”
EUGENE A. WOODS
President and CEO
Carolinas HealthCare System
2017 AHA Chair
INNOVATION
“Fostering a culture of innovation is key as the hospital field moves forward in this era of transformation. It will create novel and efficient systems of care, scientific discoveries and an improved relationship with consumers. Responsibly investing in promising ideas and technologies ultimately will improve care and affordability.”
NANCY AGEE
President and CEO
Carilion Clinic
2017 AHA Chair-Elect
Access: Coverage
Hospitals, health systems and health organizations recognize that access to health care for individuals is the cornerstone of developing healthy communities across the nation. This issue includes the topics of affordability, coverage, health equity and the widespread need for behavioral and social services. Without an adequate and appropriately trained supply of health professionals, the hospital field will not be able to meet the needs of an aging population, care for patients in rural and urban communities, address behavioral health needs and provide the breadth of services the changing health care environment will demand.
The Affordable Care Act
County-by-county analysis of current projected insurer participation in health Insurance exchanges, according to the Centers for Medicaid & Medicare Services as of September 2017.
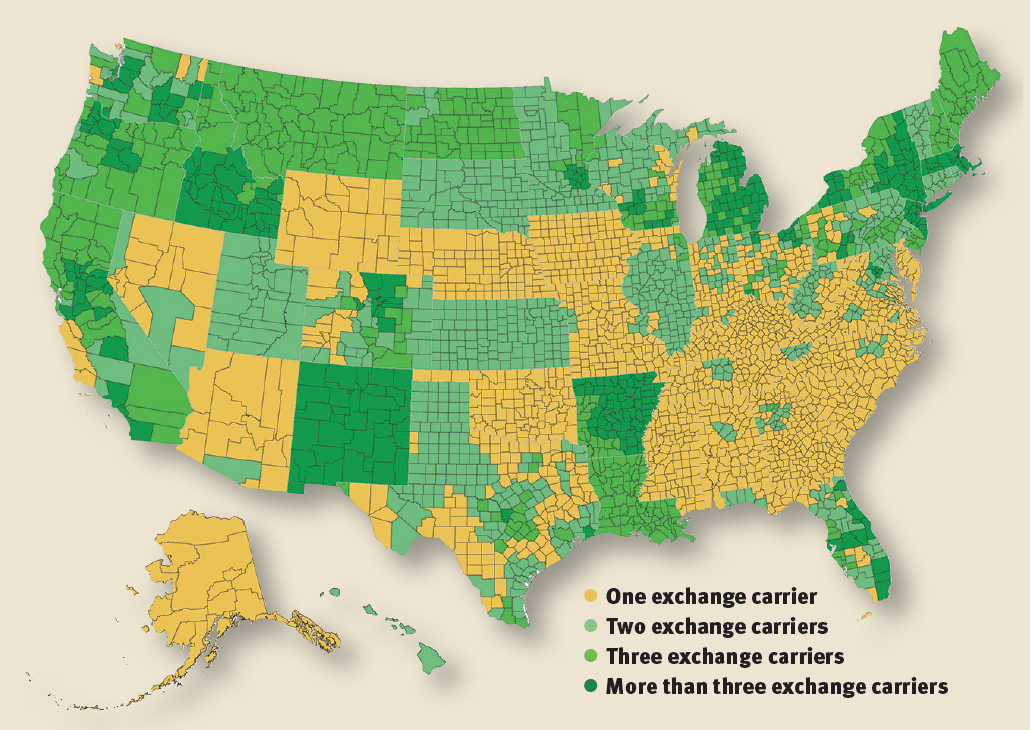
Notes: All state exchange data are self−reported from the exchanges to CMS. All data reflected on this map is a point in time as of 9/20/2017 and is expected to fluctuate. This map represents continued 2017 county-level participation in 2018 unless a carrier has publicly announced otherwise. Enrollment numbers reflected are plan selections as of the end of open enrollment, Jan. 31, 2017, and do not include enrollment in single-carrier counties for state-based exchanges.
Record low uninsured rate
- In 2016, 28.1 million people were uninsured, and the uninsured rate fell to a record low of 8.8%.(1)
- 20.5 million people have gained health insurance since 2010.(2)
Medicaid gets a big ‘thumbs up’
In 2015, Medicaid covered:
- 45% of children and 16% of adults in small towns and rural areas.(3)
- 38% of children and 15% of adults in metropolitan areas.(4)
- 62% of residents living in certified nursing facilities.(5)
- One in 10 veterans.(6)
Medicaid support
The majority of the public — regardless of partisanship — hold favorable views of Medicaid, the government health insurance and long-term care program for low-income adults and children. Surveys show that 74% have a favorable view of Medicaid. Only 1/3 of the public support reducing funding for Medicaid expansion or limiting how much money each state gets from the federal government.(4)
 Cost-Sharing Reduction (CSR) payments
Cost-Sharing Reduction (CSR) payments
- CSR payments, federal government payments that help to lower co-pays and deductibles for low-income Americans who earn between 100 and 250% of the federal poverty level, will total $7 billion this year if they are all made.(7)
- About 12 million people bought health insurance through the ACA’s insurance markets for 2017, and 7 million of them (58%) qualified for CSR payments.(8)
If the CSR payments are halted:
- Silver plan gross premiums, before accounting for tax credits, will rise by 20% in 2018, and 25% by 2020. Silver plans are one of 4 categories of marketplace plans and are the most common choice among consumers.
- The federal deficit would increase, on net, by $194 billion from 2017 through 2026.(9)
- More than 70% of voters support help with out-of-pocket health care costs such as deductibles and co-pays.(10)
Access: Workforce
Nursing challenges remain
- 1.2 million vacancies will open up for registered nurses between 2014 and 2022.(11) A combination of an aging patient population and the retirement of nurses contribute to this trend.(12)
- The Nurse Licensure Compact allows nurses to have one multistate license, with the ability to practice in both their home state and other compact states. 25 states have joined the compact. This program can facilitate telenursing.(13)
 Physician shortage looms
Physician shortage looms
- 49% of physicians often or always experience feelings of burnout.(14)
- 21% of physicians’ time is spent on non clinical paperwork, the equivalent of 168,000 physician FTEs not engaged in clinical activities.(14)
- The nation faces a shortage of between 40,800 and 104,900 physicians by 2030.(15)
- First-year enrollment at U.S. medical schools has increased by 28% since 2002, with 22 new schools accounting for nearly 40% of the growth.(14)
- ACGME-accredited, entry-level residency positions are continuing to grow at a rate of about 1% per year. Federal caps on Medicare-funded residency training positions remain effectively frozen at 1996 levels.(15)
Futurescan Prediction
More than half (58%) of hospital executives consider it very likely that by 2022 their hospital will have implemented strategies to increase employee job satisfaction and “joy in work,” and another 37% think it somewhat likely.(16)
Access: Affordability
Affordability plays a key role in advancing access to health care, and community and legislative efforts increasingly focus on this issue.
 Drug prices are skyrocketing
Drug prices are skyrocketing
Total annual spending on prescription drugs has reached $309 billion, the fastest growing segment of the U.S. health care economy. The price of drugs, not utilization, is the predominant contributor to the increase. (17)
- 38.7% growth in inpatient drug spending on a per admission basis over a two-year period.
- More than 90% of hospitals said spending on pharmaceuticals was of moderate or severe concern.
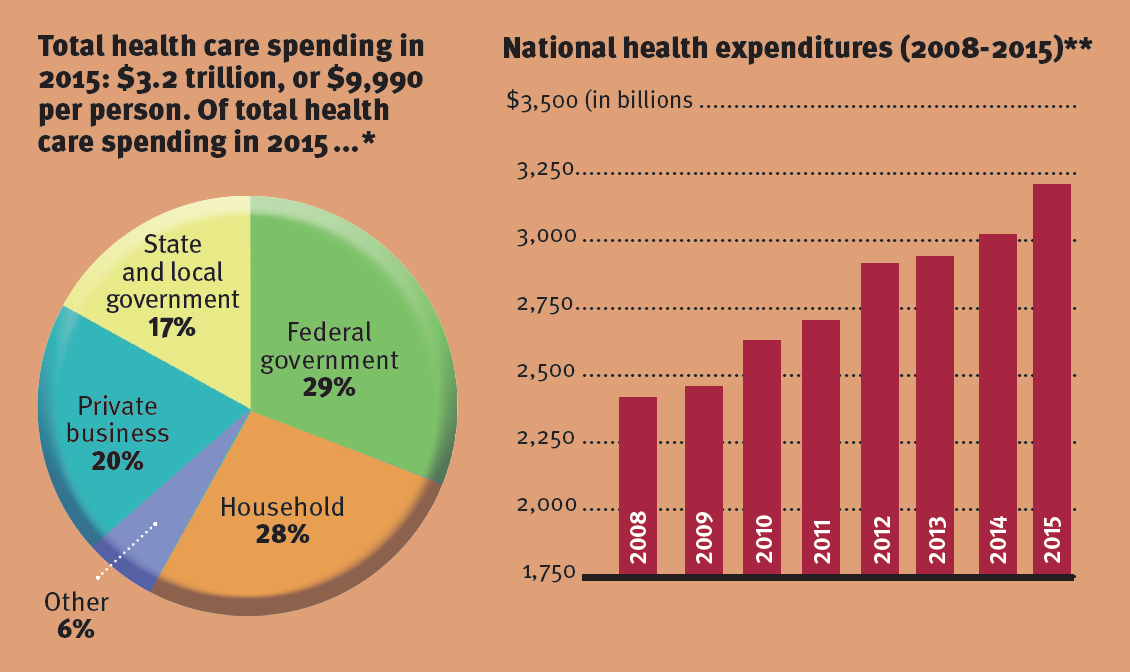
Total U.S. health care spending on the rise
Total U.S. health care spending in 2015 grew by 5.8 %, the fastest rate increase since 2007.
- Total health care spending in 2015: $3.2 trillion, or $9,990 per person. Of total health care spending in 2015...(18)
Disparities in health care
Health disparities add significant costs for the U.S. health care system. The total cost of racial/ethnic disparities in 2009 was $82 billion.(19) Below are the projections if disparities remain unchanged:
- 2009 - $82 Billion
- 2020 - $126 Billion
- 2050 - $353 Billion
Consumers are worried about affordability
Four in 10 (43%) adults with health insurance say they have difficulty affording their deductible, and roughly a third say they have trouble affording their premiums and other cost sharing; all shares have increased since 2015.
Three in 10 (29%) Americans report problems paying medical bills. Of this group, seven in 10 (73%) report cutting back spending on food, clothing or basic household items.
Half of the public says they are at least somewhat worried they won’t be able to afford needed health care services.(20)
National health expenditures will nearly double by 2025
$2.9 trillion in 2013 to $5.5 trillion in 2025, a rate that will outpace national gross domestic product by 1.2% per year during this period.(21)
However, hospitals have done significant work to control costs
- The annual growth in hospital prices has slowed in comparison to the previous year in nine of the past 10 years.
- The annual percentage change in hospital prices (both inpatient and outpatient): 1.2% — 2016, compared with 4.4% — 2006.(22)
High deductibles and HSAs
In employer-sponsored health insurance plans, the combination of a high-deductible health plan and a Health Savings Account increases affordability pressure.(23)
- In 2015, 24% of all workers were enrolled in a high-deductible plan.
- Within the next three years, 44% of employers are expected to offer high-deductible plans as the only option.(24)

The Middle Class
Middle-income households’ spending on health care has increased 25% since 2007. Spending on other basic needs, such as food and clothing, has decreased.(25)
FUTURESCAN INSIGHT
In the 2017 Futurescan survey of hospital executives, nearly 60% indicated that the federal government’s effort to reduce health care spending is among the top factors that concern them most about health care affordability, and 50% cited growing premiums and out-of-pocket medical expenses for patients.(26)
Access: BEHAVIORAL HEALTH
 The drug and opioid crisis
The drug and opioid crisis
- Drug overdoses are now the leading cause of death among Americans younger than 50. In 2016, they exceeded 59,000, a 19% increase from 2015.(27)
- Since 1999, the amount of prescription opioids sold in the U.S. nearly quadrupled, yet there has not been an overall change in the amount of pain that Americans report.(28)
- 180% Physicians’ and other health care professionals’ registrations with state-based prescription drug monitoring programs grew 180%. There were 471,896 enrolled in 2014. That number grew to 1,322,996 in 2016.(29)
The majority of drug overdose deaths (more than six out of 10) involve an opioid.(28)
Mental health issues continue
- Only 41% of adults in the U.S. with a mental health condition received mental health services in the past year.
- African-Americans and Hispanic-Americans used mental health services at about one-half the rate of Caucasian-Americans and at about one-third the rate of Asian-Americans.
- Serious mental illness costs America $193.2 billion in lost earnings per year.
- One in five adults in the U.S. — 43.8 million, or 18.5% — experiences MENTAL ILLNESS in a given year.(30)
A workforce shortage in behavioral health
- There is one licensed psychiatrist for every 30,000 people in the U.S., with a projected 10% decrease in the clinician population over the next decade.(31)
- 85% of federally designated behavioral health professional shortage areas are in rural locations.(32)
- Between 2004 and 2014, the number of telemental health visits by rural beneficiaries grew on average 45.1 % annually, according to an analysis of Medicare fee-for-service claims.(33)
Value: Health care transformation and value-based care models focusing on populations can improve the quality of care at a lower cost.
 Value-based care
Value-based care
- The financial incentives in the Medicare Access and CHIP Reauthorization Act will accelerate the transition to alternative payment models not only in the public sector, but also in the private sector.
- Value-based insurance design will speed patients’ understanding of the variation in cost and quality of services among providers.
- Providers need the infrastructure to monitor their quality and financial performance in near-real time, so they can afford to take on risk. Currently, many providers do not have the information they need to manage that risk successfully.(34)
Analytics and quality
Global hospital expenditures on analytics are anticipated to reach $18.7 billion by 2020, up from $5.8 billion in 2015, as hospitals focus on quality and cost reduction.(35)
Non-value added treatments
Excessive testing and treatment costs $200 billion annually. This overly aggressive testing can also harm patients, generating mistakes and injuries believed to cause 30,000 deaths each year. (36)
 Health care leaders’ perspective
Health care leaders’ perspective
- 66% say their organizations are fully committed and underway with the transition to value-based care or have experimental or pilot programs.
- 65% of CEOs view shared-risk models as an opportunity.(37)
Bundled payments reduced Medicare payments
In the first 21 months of the Bundled Payments for Care Improvement Initiative (BPCI), Medicare payments declined more for lower extremity, joint-replacement episodes provided in BPCI-participating hospitals than for those provided in comparison hospitals, without a significant change in quality outcomes.(38)
Quality improvement
21% decline in hospital-acquired conditions from 2010 to 2015:
- 125,000 lives saved.
- $28.2 billion in cost savings.(39)
Results from a clinical trial using hard surfaces and linens infused with copper-oxide compounds:
- 78% overall reduction in multidrug-resistant organisms in a real-world clinical environment. This could prove to reduce health care-associated infections.(40)
Results from a nurse-led quality improvement program addressing malnutrition among hospitalized patients:
- Decrease in hospital-acquired conditions.
- Shorter length of stay.
- Lower readmission rates.
- Reduced cost of care.(41)
FUTURESCAN INSIGHT
More than half (55%) of hospital executives consider it very likely that by 2022 their hospital will have achieved improvements in value metrics (such as better patient outcomes, greater capacity, or reduced
costs) through telemedicine and virtual healthcare solutions.(42)
Partners: Embrace diversity of individuals and serve as partners in their health
Health care providers are fostering true patient engagement and recognizing the diversity in their communities. Individuals are increasingly viewing health care through a consumer lens. As the patient grows to expect a digital health care experience, health care organizations are responding by embedding technology into care delivery and focusing on protecting patient information.
 Patient engagement continues to rise
Patient engagement continues to rise
- 70% of patients say they have become more engaged with their health care during the past two years, up from 57% in 2016. The top two drivers are greater access to personal health records and online patient portals.
- 71% of providers say patient engagement is a top priority at their organizations, up from 60% in 2016. The top drivers are technology advancements and meaningful use requirements, both important to improving overall care.
- 95% of patients experience benefits from engagement with their personal health care information online. Benefits include becoming more knowledgeable about personal medical information and saving time.
- Providers say online patient portals have improved overall patient care, improved records tracking and increased office efficiency.(43)
Consumerism
- Over the past 10 years, two different purchaser trends — increased patient cost sharing at the point of service and a shift to outcomes-based payment — have converged to catalyze a movement toward consumerism in the health care field.
- Health plans and providers both will be increasingly responsible for providing the education, information and tools that consumers need to take ownership of their health. (44)
Letting patients type PRE-VISIT AGENDAS INTO THE ELECTRONIC HEALTH RECORD SYSTEM before seeing the physician made appointments more efficient, improved clinicians’ preparedness and improved communication.(45)
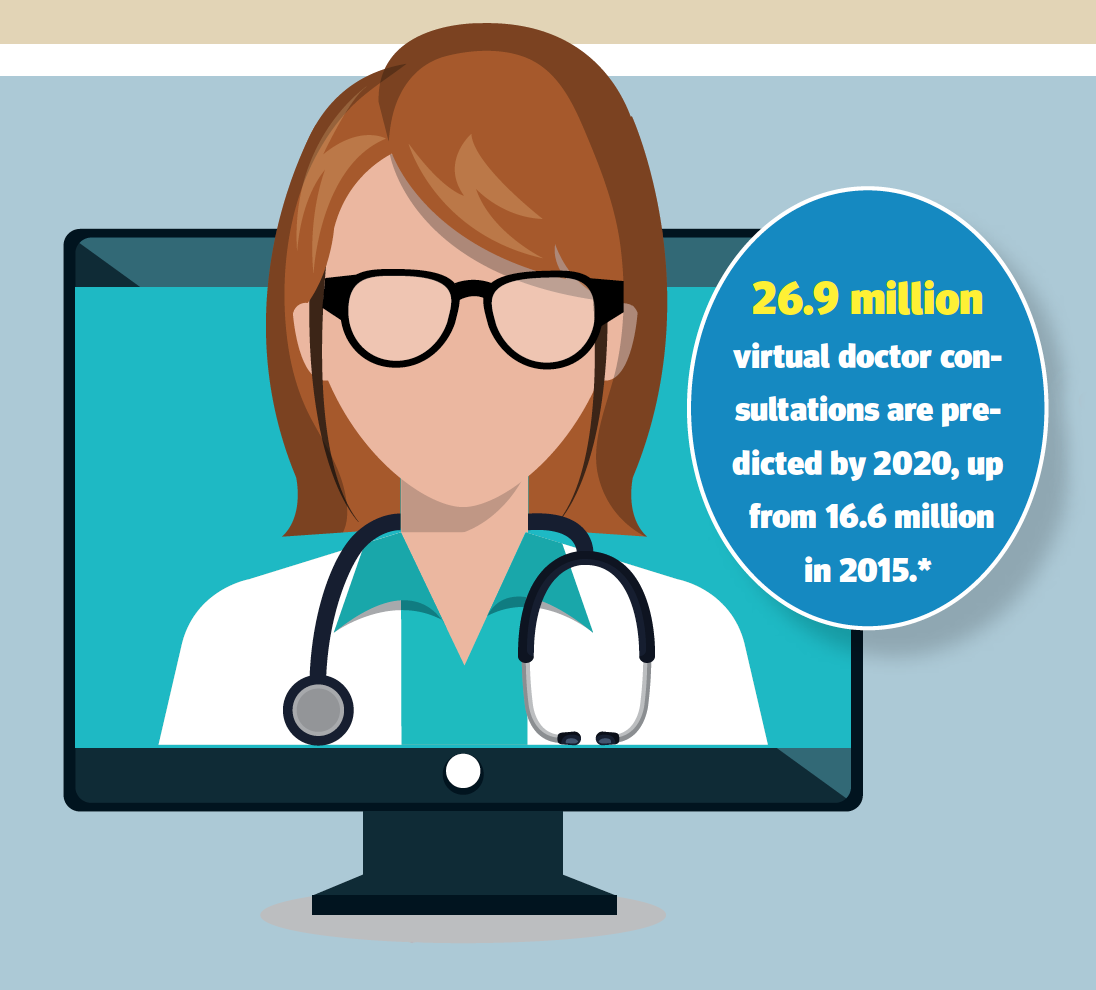 Telemedicine’s rapid growth
Telemedicine’s rapid growth
- 78% of consumers say they would be interested in receiving health care virtually some or most of the time.(46)
- 35% of employers offer telemedicine services on-site, which is expected to surpass 47% in the coming year. The global telemedicine market is expected to grow at a com-pound annual rate of 14.3%, more than doubling it from 2014 to 2020.(47)
- Remote monitoring and other technology-enabled care delivered at or near a patient’s home will become standard practice in the foreseeable future. Health systems that cannot provide such care will be at a competitive disadvantage.(48)
- 26.9 million virtual doctor consultations are predicted by 2020, up from 16.6 million in 2015.(46)
Cybersecurity remains a hot topic
- More than eight in 10 U.S. health care organizations will increase security spending in 2017.(49)
- One in five U.S. health care survey respondents had experienced a data breach in 2016, compared with the global average of 26%.(49)
- Data breaches cost the health care field approximately $6.2 billion each year, with the average breach incurring damages of $2.2 million and compromising 3,128 records per incident.(50)
- Although more records were breached in 2015 than in 2016, 2016 saw a greater number of breaches, the largest of which predominantly impacted provider organizations.(50)
- 67% of medical device manufacturers and 56% of health care delivery organizations think an attack is likely to occur within a year on a medical device they use.(51)
Health care organizations are most concerned about:
- Ransomware 69%(50)
- Phishing Attacks 61%(50)
- Negligent Insiders 55%(50)
Diversity in your patients, workforce
- To improve health equity, organizations first need to understand where disparities exist. This requires the accurate collection of race, ethnicity and language data, along with the resources to analyze it.(52)
- As patient populations become increasingly diverse, providing culturally competent care is more important than ever. The changing composition of staff provides leaders with unique capabilities that can be leveraged to tailor care experiences so that they are more effective and appropriate. Recent research shows that more racially and ethnically diverse companies out perform other organizations financially.(53)
Health ownership by consumers
Three key dimensions can lead to a state of mind of “health ownership” for the consumer:
- A deeper and more sustainable motivation to achieve or maintain good health.
- Better decision-making —choosing high-value providers for the appropriate services.
- Expectations of a better experience.(54)
FUTURESCAN INSIGHT
By 2021, 99% of hospital executives think it at least somewhat likely that patients in their hospitals will demand a greater role in the planning of their treatment.(53)
Well-Being: Focus on well-being and partnership with community resources
The health care system is evolving outside of the four walls of the hospital and into the community in an effort to manage and prevent chronic disease and improve the well-being of patients and the community.
Chronic diseases are driving up health care spending
- 86% of the nation’s health care spending is for patients with one or more chronic conditions.(55)
Diabetes
- 54.9 million people will have diabetes in the U.S. in the year 2030, compared with 35.6 million in 2015. This represents a 54% increase.
- Diabetes will cost the nation more than $622 billion in 2030, up from roughly $408 billion in 2015.(56)
Alzheimer’s disease
- The number of Americans 65 or older with Alzheimer’s disease is projected to increase from 5.1 million in 2015 to 13.5 million in 2050.
- The cost of care will rise from $113 billion in 2015 to $589 billion in 2050, and will represent nearly one in three Medicare dollars.(57)
 Seniors and their chronic conditions
Seniors and their chronic conditions
- 25% of seniors on Medicare have four or more chronic conditions.
- Individuals with chronic conditions account for 93% of total Medicare spending.
Among beneficiaries with six or more chronic conditions:
- One-quarter had made at least three visits annually to the emergency department.
- Two-thirds had been hospitalized.
- Nearly half required a post-acute care stay.(58)
Outpatient facilities
Hospitals are investing more in outpatient facilities, from full-scale service centers to urgent care centers to stand-alone emergency departments.(59)
- Outpatient revenue increased from 28% in 1994 to 47% in 2015
- Inpatient revenue decreased from 72% in 1994 to 53% in 2015(60)
High-need patients toll
(Adults with two or more major chronic conditions)
- 71% of the nation’s health care spending is for patients with multiple chronic conditions.(61)
- 62% of high-need patients report stress about material hardships, such as being unable to pay for housing, utilities, or nutritious meals, compared to 32% of other adults.(62)
- With better access to care and good patient–provider communication, high-need patients are less likely to delay essential care and less likely to go to the emergency department for nonurgent care, and thus less likely to accrue avoidable costs.(62)
Social determinants of health
Contribution to premature death(63)
- 40% behaviors
- 30% genetic predisposition
- 15% employment, housing, transportation and poverty
- 10% health care
- 5% environmental exposure
NUTRITION
- Nearly 40% of American adults are obese.(64)
- 24% of all Americans have at least one diet-related medical condition.(64)
Consumers want more nutritional advice from health care resources:
- 79% want advice from physicians.
- 59% want advice from pharmacies.(64)
HOUSING
- People receiving federal housing assistance from the Department of Housing and Urban Development had lower rates of uninsurance and unmet medical need due to cost, compared with that of a control group.(65)
VIOLENCE
Proactive and reactive violence response efforts cost U.S. hospitals and health systems $2.7 billion in 2016. This includes:
- $280 million related to preparedness and prevention to address community violence.
- $852 million in unreimbursed medical care for victims of violence.
- $1.1 billion in security and training costs to prevent violence within hospitals.
- $429 million in medical care, staffing, indemnity and other costs as a result of violence against hospital employees.(66)
 20% of the U.S. population lives in what is considered a RURAL AREA, and patients in these areas are more likely to have multiple chronic illnesses and higher mortality rates.(67)
20% of the U.S. population lives in what is considered a RURAL AREA, and patients in these areas are more likely to have multiple chronic illnesses and higher mortality rates.(67)
FUTURESCAN INSIGHT
[ EXPERT INSIGHT ]
“To succeed in providing holistic care for individuals, we must increase our efforts to meet patients where they are and make it simpler and more convenient for them to become and stay healthy.”
— Howard R. Grant, M.D., J.D. (p. 25)(68)
[ SURVEY INSIGHT ]
By 2021, 47% of hospital executives believe most insured patients will belong to health plans that pay beneficiaries for meeting certain health targets, such as healthy blood pressure.(69)
Coordination: Seamless care propelled by teams, technology, innovation and data
Better care coordination will organize patient care activities and information in an efficient and effective manner to achieve safer care with better outcomes. Teams, technology, data and innovation will spur the advancement of care coordination throughout the continuum of the delivery system. Clinical integration is a way to provide more efficient, coordinated care, decrease costs and expand the population served by high quality medical services.
The average Medicare patient sees seven physicians across four different practices(70)
- 75% of those who are admitted to the hospital cannot identify the clinician responsible for their care.
- 20% of Medicare fee-for-service patients who are discharged from the hospital are readmitted within 30 days.
- The average primary care physician interacts with 229 physicians at 117 different practices for Medicare patients.
- Health service delivery fragmentation costs $130 billion annually.
Data and clinical decision-making(71)
- The volume of electronic health care data doubles every 24 months.
- A physician would need to spend 29 hours each workday to remain current with the latest medical literature.
- Although this massive amount of health care data is brimming with insights, organizations are struggling to unlock its full value.
- Leaders will need to adopt sophisticated systems that support and enhance decision-making in clinical settings and that enable success in risk-based payment arrangements.
TeamSTEPPS® shows results
TeamSTEPPS® is an evidence-based set of teamwork tools aimed at optimizing patient outcomes by improving communication and team-work skills among health care professionals. After implementing a discharge intervention incorporating TeamSTEPPS® principles:(72)
- Length of stay was reduced, providing cost savings to the hospital.
- Patient satisfaction improved.
- Readmission rates improved.
Electronic health records
The proprietary nature and standards for electronic health records likely will diminish, as field pressure opens up data repositories and personal data become more accessible.(73)
- 2004 — one in five physicians used an electronic health record; today — nine in 10 physicians.
- 9 in 10 physicians use an electronic health record in their practices.
 Execs’ smartphone and tablet usage
Execs’ smartphone and tablet usage
A study of C-suite executives, IT professionals, clinicians and department heads:(74)
- 79.8% use tablets and 42.6% use smartphones to access the information needed to provide and coordinate care.
Interoperability and privacy
All stakeholders must work with consumer groups to develop a protocol for unique patient identifiers that balance the societal expectation of privacy with the need to provide caregivers with potentially lifesaving comprehensive patient clinical data. This will help to achieve true data interoperability across electronic health record platforms.(75)
Physician practice consolidation
The trend toward consolidation of physician practices in recent decades is accelerating. The proportion of physicians in groups of nine or fewer dropped from 40.1% in 2013 to 35.3% in 2015, while the proportion of those in groups of 100 or more increased from 29.6% to 35.1% during the same period.(76)
Hospital field realignment
Between 2010 and 2015, the number of announced hospital mergers and acquisitions increased by 70%. This recent history, along with future demands, suggests that consolidations will continue. More affiliations between traditional and nontraditional organizations will take place. Hospitals get rapid access to new capabilities, while nontraditional provider organizations get rapid access to larger patient populations.(77)
Recent hospital mergers have:(78)
- Decreased costs — 1.5% reduction in annual operating expenses as acquired hospitals.
- Decreased capital and operating costs.
- Improved clinical standardization.
- Improved outcomes for patients and reduced readmission rates.
FUTURESCAN INSIGHT
By 2022, 51% of hospital executives think it very likely that their hospital will implement secure, HIPAA-enabled cloud technology to promote collaboration and information sharing across the organization and among providers, regardless of location. Almost half (48%) of respondents think it very likely that physicians and other caregivers at their hospital will have access to computer-generated optimal care pathways for individual patients, based on the patient’s data and longitudinal data from comparable patients.(79)
Innovation:
Innovation can drive improvements in care coordination and the transformation of the health care delivery system. Additionally, innovation activities can make health care more efficient and will play a key role in addressing the issue of affordability.
Investment in innovation
- In 2015, a record $16.1 billion in venture capital funding was invested in U.S. health care companies.(80)
- Of that, $4.5 billion was invested in companies designing consumer-engagement tools and wearable devices.(80)
Advice from investors regarding telehealth:
- Think about how telehealth integrates into consumer solutions.
- Focus on how telehealth tools change the delivery system and sites of service.
- Major specialty growth areas within telehealth are tele-ICU, telestroke, and telebehavioral health.
- Platforms that manage particular high-utilization populations, like those with chronic care conditions, provide growth opportunities.(81)
Health care leaders’ top investment areas over the next three years:
- Data Aanalytics 71%
- Career Redesign Efforts 65%
- Patient Experience Improvement 61%
- Care Coordination 60%(82)
Disruptive innovation
According to health care executives, clinical leaders and clinicians:(83)
- 54% say that disruptive innovation for hospitals and health systems will come from startups.
- 65% say hospitals and health systems are a health care sector most in need of disruptive innovation.
- 47% say health care IT is a health care sector most in need of disruptive innovation.
- 36% say primary care is a health care sector most in need of disruptive innovation.
Top 10 Innovations to achieve more for less in health care(84)
- Next-generation gene sequencing
- 3-D printing of medical devices
- Immunotherapy
- Artificial intelligence
- Point-of-care diagnostics
- Virtual reality Leveraging social media to improve patient experience
- Biosensors and trackers
- Convenient care
- Telehealth
 Innovation centers
Innovation centers
Many health care organizations have established innovation centers to coordinate previously disjointed efforts. These centers have a median staff of six and a median annual budget of $1.9 million, although staff and funding vary widely.(85)
Retailers and tech companies are moving into health care
More retailers and technology companies are getting involved in health care innovation. More than 90 startup companies are working on artificial intelligence applications in health care.(86) Algorithms analyze patients’ health, diagnose problems and design optimal personalized treatment plans.
The IBM Watson cognitive computing system:
- Reads 40 million documents in 15 seconds.
- Ingests an average of 27,000 new documents per day.
- Has a 90% successful diagnosis rate for lung cancer.(87)
Google Brain is applying its machine-learning expertise and working with hospitals to predict health outcomes from deidentified medical data.(88)
CVS Health has 50% of the retail clinic market share.
- 27% of emergency department visits could be handled at retail clinics and urgent care centers at a cost savings of about $4.4 billion per year.(89)
Warby Parker will start to offer online vision tests. (90)
CEO perspective
- Innovation is not limited to technology or bioscience, but extends across all aspects of operations. CEOs have to act and think differently to lead their organizations during this time of industry change.
- Regulatory uncertainty creates a vacuum that innovation will fill. Incumbent health systems have advantages in driving transformation — but if they don’t act, others will.
- Not all innovations are created equal. Transformative innovation delivers better value as measured by outcomes, prices and customer experience.(91)
3-D printing
- By 2019, 10% of people in the developed world will be living with 3-D printed items on or in their bodies.
- By 2019, 3-D printing will be a central tool in more than one-third of surgical procedures involving prosthetics and implanted devices.
- The overall market for medical 3-D printing is expected to grow to $1.21 billion by 2020 from about $660 million in 2016.(92)
FUTURESCAN INSIGHT
Hospitals recognize that innovation is a leadership imperative; 91% of survey respondents say it is at least somewhat likely that by 2022, one of their hospital’s strategic objectives will be to increase the innovation skills of its leadership.(93)
Q&A: Maryjane Wurth
How is the American Hospital Association anticipating the future in this era of uncertainty and rapid change?
The AHA is well-prepared to assist the hospital field by addressing the many scenarios that could come to fruition in the coming years. We have embedded the strategies of Advocacy and Representation, Thought Leadership, Knowledge Exchange and Change Agency throughout our programs and services. Through these approaches, we have crafted an innovation strategy across the AHA to accelerate health care’s transformation to new delivery and payment models and address affordability. We also have a leadership team devoted to innovative solutions and partnerships so we can rapidly respond to opportunities and challenges in the environment. Our innovation strategy involves the advancement of data-driven solutions to provide field-leading information, individualized member experiences, proactive analytics and tools that support our members. These strategies will complement and amplify our advocacy efforts.
What does health care leadership look like in this volatile environment?
Leaders in health care need to assess the realities of their particular situations, and balance their current circumstances with the need to envision and prepare for the future. This will entail asking pertinent questions, looking for new solutions, supporting a nimble environment, and being receptive to new partnerships and models of care delivery. Leaders have to rely on their teams, including governance, management, clinicians and staff, to develop and implement these solutions. This will require dedication of resources to substantial communication, training and culture change. Find and nurture the champions of new approaches in your organization who can then spread the word to colleagues. Always remember to ground your programs and services in the mission and purpose of your organization. And remember to celebrate successes and tell your story as it evolves — this provides inspiration to your employees and affirms the important role hospitals and health systems play in the community.
In terms of advocacy, we are living in a time when there is no clear federal vision for health care in America. Health care leaders are courageously stepping up in this vacuum to actively shape the future. We need our leaders to continue to use their voices and mobilize their stakeholders and employees to influence efforts in the interest of patients and the communities we serve.
Maryjane Wurth is Executive Vice President and Chief Operating Officer of the American Hospital Association and President and CEO of Health Forum
Hospitals and health systems: The economic engine of communities
Hospitals, including their ripple effect, support:
- 16 million total jobs, or one of nine jobs, in the U.S.
- More than $2.8 trillion in economic activity.(94)
Based on current hiring trends, health care will become the nation’s largest sector by 2019, passing the entire retail sector.(95)
The AHA Strategic Plan
The AHA strategic plan provides the framework to carry out the mission to advance the health of individuals and communities. The AHA leads, represents and serves hospitals, health systems and other related organizations that are accountable to the community and committed to health improvement. To view the plan, visit www.aha.org/strategy.
Our Commitments
Hospitals and health systems are committed to these five essential elements that form the core of the AHA’s vision of a society of healthy communities where all individuals reach their highest potential for health.
- Access – Access to affordable, equitable health, behavioral and social services
- Value – The best care that adds value to lives
- Partners – Embracing diversity of individuals and serve as partners in their health
- Well-being – Focus on well-being and partnership with community resources
- Coordination – Seamless care propelled by teams, technology, innovation and data
Fostering Advancements for Members and the Field
Just as hospitals and health systems are undergoing transformation, the AHA is also changing to meet the needs of our members and to proactively explore trends of the future. Working with our membership and other stakeholders, the AHA is focused on providing value, guidance and forward-thinking solutions through the key strategies of:
- Knowledge Exchange
- Advocacy and Representation
- Agent of Change
- Thought Leadership
- American Hospital Association
- AHA Members and Stakeholders
Resources
- “Uninsured Rate Falls to Record Low of 8.8%,” Phil Galewitz, Kaiser Health News, Sept. 12, 2017
- “Feds estimate 50.5 million more people with insurance since Obamacare became law,” Robert King, Washington Examiner, Aug. 29, 2017.
- “Medicaid in Small Towns and Rural America: A Lifeline for Children, Families and Communities,” Georgetown
University Center for Children and Families, and the North Carolina NC Rural Health Research Program, June 2017 - “Kaiser Health Tracking Poll — June 2017: ACA, Replacement Plan, and Medicaid,” Ashley Kirzinger et al., Kaiser Family Foundation, KFF.org, June 23, 2017
- “Distribution of Certified Nursing Facility Residents by Primary Payer Source,” Kaiser Family Foundation, KFF.org
- “Fact Sheet: Cutting Medicaid Would Hurt Veterans,” Families USA, May 2017
- “Senate to hold bipartisan hearings to stabilize Insurance Markets,” NPR WBEZ, Alison Kodjak, Aug. 1, 2017
- “Essential Facts About Health Reform Alternatives: Eliminating Cost-Sharing Reductions,” The Commonwealth Fund, www.commonwealthfund.org, August 21, 2017
- “The Effects of Terminating Payments for Cost-Sharing Reductions,” Congressional Budget Office, www.cbo.gov, August 2017
- Infographic: American Benefits Council, www.americanbenefitscouncil.org, March 2017
- “Nearly half of nurses consider changing careers as nationwide shortage looms, RNnetwork study says,” Beth Jones Sanborn, Healthcare Finance, March 1, 2017
- “U.S. still headed for nurse shortage,” Sally Jimenez, Nurse.com, Feb. 16, 2016
- Nurse Licensure Compact website: www.nursecompact.com
- “2016 Survey of America’s Physicians: Practice Patterns & Perspectives,” The Physicians Foundation, September 2016
- “Results of the 2016 Medical School Enrollment Survey,” Association of American Medical Colleges, 2017
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for Healthcare Strategy & Market Development, 2017
- Infographic “A Dose of Facts,” Federation of American Hospitals and the American Hospital Association, 2016
- “National Health Spending: Faster Growth In 2015 As Coverage Expands And Utilization Increases.” Anne B. Martin, et al. Health Affairs (2016): 10-1377 — from RPB PPT
- "Medical Cost Trend: Behind the Numbers 2016", PWC, 2015
- “Data note: Americans’ Challenges with Health Care Costs,” Bianca DiJulio et al., Kaiser Family Foundation KFF.org, March 2, 2017
- “Emergency Health Care Professionals’ Understanding of the Costs of Care in the Emergency Department,” Kevin A. Hoffman, DO, Michelino Mancini, D.O., The Journal of the American Osteopathic Association, June 2017, Vol. 117, 359-364
- Bureau of Labor Statistics. Producer Price Index data, 2006 -2016, for Hospitals (NAICS Code 622)
- “The Financial Burdens Of High-Deductible Plans,” Salam Abdus, Thomas M. Selden and Patricia Keenan, Health Affairs 35, no.12 (2016):2297-2301, doi: 10.1377/hlthaff.2016.0842
- “Health Care 2020: Consumerism,” Healthcare Financial Management Association, 2016
- “Burden of Health-Care Costs Moves to the Middle Class,” Anna Louie Sussman, The Wall Street Journal, Aug. 25, 2016
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for Healthcare Strategy & Market Development, 2017
- “Drug Deaths in America Are Rising Faster Than Ever,” Josh Katz, The New York Times, June 5, 2017
- “Drug overdose deaths in the United States continue to increase in 2015,” CDC.gov/drugoverdose/epidemic/index.html, 2017
- “Physicians’ progress to reverse the nation’s opioid epidemic,” American Medical Association, 2017
- “Mental Health By the Numbers,” National Alliance on Mental Illness – www.nami.org, 2017
- “Telehealth Providers Make a Play for Online Psychiatry Services,” Eric Wicklund, mHealth Intelligence, Sept. 20, 2016
- The State of the Behavioral Health Workforce: A Literature Review,” American Hospital Association. http://www.aha.org/content/16/stateofbehavior.pdf, 2016
- “Rapid Growth In Mental Health Telemedicine Use Among Rural Medicare Beneficiaries, Wide Variation Across States,” Ateev Mehrotra, et al., Health Affairs 36, no.5 (2017):909-917
- “Health Care 2020: Transition to Value,” Healthcare Financial Management Association, 2016
- “2017 global health care sector outlook: Making progress against persistent challenges,” Rebecca George, Deloitte University Press
- “Putting A Lid On Waste: Needless Medical Tests Not Only Cost $200B — They Can Do Harm,” Chad Terhune, Kaiser Health News, May 24, 2017
- “Annual Industry Outlook: The Road to Value-Based Care,” HealthLeaders Media. January/February 2017.
- “Association Between Hospital Participation in a Medicare Bundled Payment Initiative and Payments and Quality Outcomes for Lower Extremity Joint Replacement Episodes,” Laura A. Dummit, MSPH, et al., Journal of the American Medical association, Sept. 19, 2016
- “National Scorecard on Rates of Hospital-Acquired Conditions 2010 to 2015: Interim Data From National Efforts To Make Health Care Safer,” www.ahrq.gov/professionals/quality-patient-safety/pfp/2015-interim.html
- “Health system deploys copper-infused surfaces to decrease infections,” Jamie Morgan, Health Facilities Management, March 28, 2017
- “Health System Quality Improvement: Impact of Prompt Nutrition Care on Patient Outcomes and Health Care Costs,” Anita Meehan et al., Journal of Nursing Care Quality, 31(3): 217-223, July-September 2016
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for Healthcare Strategy & Market Development, 2017
- “2017 Patient Engagement Perspectives Study,” CDW, February 2017
- “Health Care 2020: Consumerism,” Healthcare Financial Management Association, 2016
- “78% of Physicians ‘More Prepared’ When Patients Enter EHR Notes Ahead of Appointments,” Alexandra Wilson Pecci, HealthLeaders Media, April 4, 2017
- “Are You Meeting the Rising Demand for Virtual Care? Get the Facts,” Carenet Healthcare Services, April 25, 2017
- “2017 Healthcare Talent Scan,” American Hospital Association, 2017
- “Health Care 2020: Transition to Value,” Healthcare Financial Management Association, 2016
- “2017 Thales Data Threat Report: Trends in Encryption and Data Security,” Research Brief, Thales eSecurity, 2017
- “The Rampant Growth of Cybercrime in Healthcare,” Issue Brief, Workgroup for Electronic Data Interchange, March 20, 2017
- “Synopsys and Ponemon Study Highlights Critical Security Deficiencies in Medical Devices,” Synopsys Inc., May 25, 2017
- “Achieving Health Equity: A Guide for Health Care Organizations,” R. Wyatt et al., IHI white paper. Institute for Healthcare Improvement, 2016
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for the Healthcare Strategy & Market Development, 2017
- “Health Care 2020: Consumerism,” Healthcare Financial Management Association, 2016
- “Multiple Chronic Conditions Chartbook: 2010 Medical Expenditure Panel Survey Data,” Jessie Gerteis, MPH et al., Agency for Healthcare Research and Quality, April 2014
- “Diabetes 2030: Insights from Yesterday, Today, and Future Trends,” William R. Rowley, M.D., et al., Population Health Management, Feb. 1, 2017
- Changing the Trajectory of Alzheimer’s Disease: How a Treatment by 2025 Saves Lives and Dollars,” Alzheimer’s Association, 2015
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for Healthcare Strategy & Market Development, 2017
- “Changing priorities shift hospital focus to outpatient strategies,” Jennifer Zaino, Healthcare Finance, Aug. 25, 2014
- “AHA TrendWatch Key Statistics for Hospitals,” American Hospital Association, May 2017
- “Multiple Chronic Conditions Chartbook: 2010 Medical Expenditure Panel Survey Data,” Jessie Gerteis, MPH et al., Agency for Healthcare Research and Quality, April 2014
- Issue Brief “How High-Need Patients Experience Health Care in the United States,” Jamie Ryan et al., The Commonwealth Fund, December 2016
- “Achieving Health Equity: A Guide for Health Care Organizations.” R. Wyatt et al., IHI white paper. Institute for Healthcare Improvements, 2016
- “Top health industry issues of 2017: A year of uncertainty and opportunity,” PWC’s Health Research Institute, December 2016
- “Datagraphic — Health Equity,” Health Affairs, June 2017
- Cost of community violence to hospitals and health systems,” Jill Van Den Bos et al., Milliman Research Report, July 26, 2017
- “The Imperative for Strategic Workforce Planning and Development: Challenges and Opportunities,” http://www.aha.org/content/17/cpi-report.pdf
- Futurescan 2017-2022: Healthcare Trends and Implications, Society for AHA’s Healthcare Strategy & Market Development, 2017
- Futurescan 2016-2021: Healthcare Trends and Implications, Society for AHA’s Healthcare Strategy & Market Development, 2016
- “Bright Spots in Care Management in Medicare Advantage,” Robert Graham Center Policy Studies in Family Medicine and Primary Care,” June 2017
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for the Healthcare Strategy & Market Development, 2017
- Lisanne Catherine Cruz, et al. “Barriers to discharge from inpatient rehabilitation: a teamwork approach.” International Journal of Health Care Quality Assurance, Vol. 30, No. 2: 137-147, 2017
- 3 Health Care Trends That Don’t Hinge on the ACA, F. Baitman and K. Karpay, Harvard Business Review, May 25, 2017
- “Healthcare pros increasingly using tablets, smartphones for job functions,” Bill Siwicki, Healthcare IT News, March 31, 2017
- “Health Care 2020: Transition to Value,” Healthcare Financial Management Association, 2016
- “Consolidation of U.S. Physician Practices Continues to Surge,” Nicola M. Parry, D.V.M., Medscape Medical News, Sept. 7, 2016
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for the Healthcare Strategy & Market Development, 2017
- “Hospital Merger Benefits: Views from Hospital Leaders and Econometric Analysis,” Monica Noether, Ph.D., and Sean May, Ph.D., Charles River Associates, January 2017
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for Healthcare Strategy & Market Development, 2017
- “Health Care 2020: Transformative Innovation,” Healthcare Financial Management Association, 2016
- “An Investor’s Insight into Telehealth,” The National Law Review, May 3, 2017
- “Annual Industry Outlook: The Road to Value-Based Care,” HealthLeaders Media, January/February 2017
- "New Market place Survey: The Sources of Health Care Innovation," Insights Report, NEJM Catalyst, Feb. 16, 2017
- “2017 global health care sector outlook: Making progress against persistent challenges,” Deloitte
- “Health Care 2020: Transformative Innovation,” Healthcare Financial Management Association, 2016
- “10 Tech Advances That Can Change Medicine,” Eric J. Topol, M.D., Medscape Medical News, Dec. 16, 2016
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for the Healthcare Strategy & Market Development, 2017
- “Google is training computers to predict when you might get sick,” Christina Farr, CNBC.com, May 17, 2017
- “Building a Culture of Health: The Value Proposition of Retail Clinics,” Robert Wood Johnson Foundation, D. Bachrach et al., Manatt Health Solutions, ed., April 2015
- “Warby Parker Grew to $250 Million in Sales Through Disciplined Growth. Now It’s Time to Get Aggressive.” Tom Foster Inc., May 2017
- “2017 CEO Forum Report: Delivering Excellence in the New Healthcare World,” Huron Consulting Group Inc. and affiliates, Aug. 25, 2017
- “How 3-D Printing Is Changing Health Care,” Aili McConnon, The Wall Street Journal, Sept 12, 2017
- Futurescan 2017-2022: Healthcare Trends and Implications, AHA’s Society for Healthcare Strategy & Market Development, 2017
- “Hospitals are Economic Anchors in their Communities,” American Hospital Association, January 2017
- “Obamacare, the secret jobs program,” Dan Diamond, www.politico.com, July 13, 2016
Read More