B.E. Smith Team | May 09, 2018
Nurse Leaders Explore Five High-Impact Themes at AONE 2018
Under the theme of “Inspiring Leaders,” clinical executives from across the country gathered to share experiences, learn best practices, and network at the 2018 American Association of Nurse Executives (AONE) conference. It proved a rich resource for exploration, new ideas, and motivation. B.E. Smith attended the conference and shares these five themes which were a central focus in many of the sessions.
The Advantages of Building Systemness
Healthcare organizations occupy different points on the path toward an integrated, synergistic, proactive, customer focused delivery model. A model one conference session referred to as “systemness.” Nurse leaders play a critical role in building and maintaining systemness. Two sessions focused on what clinical executives can do to foster and improve integrated care, while a third provided insight into how it can be achieved.
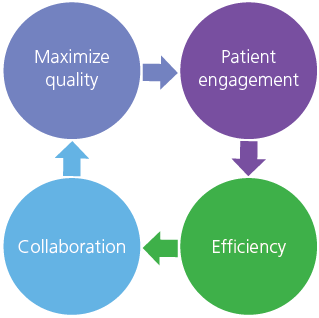 In “Transforming Interprofessional Care Delivery through Innovative Model Redesign,” North Shore University Hospital’s Dr. Margaret Duffy, Senior Administrative Director of Nursing Education, Professional Development & Research, and Ann McGrath, Senior Administrative Director of Patient Care Services, described how their system leveraged full resources on the journey to comprehensive care. The “interprofessional” approach involved “partnering skilled nurse managers with physician leaders to drive unit-level change.” Leaders empower full clinical teams to generate solutions to maximize quality, patient engagement, collaboration, and efficiency. The model’s central features are clearly defined roles for each team member, joint leader training, unit-level dashboards, and strong executive support. The result, the hospital exceeded its 2016 throughput target by 1,803 days, freeing 17 total beds while dramatically improving five key clinical measures.
In “Transforming Interprofessional Care Delivery through Innovative Model Redesign,” North Shore University Hospital’s Dr. Margaret Duffy, Senior Administrative Director of Nursing Education, Professional Development & Research, and Ann McGrath, Senior Administrative Director of Patient Care Services, described how their system leveraged full resources on the journey to comprehensive care. The “interprofessional” approach involved “partnering skilled nurse managers with physician leaders to drive unit-level change.” Leaders empower full clinical teams to generate solutions to maximize quality, patient engagement, collaboration, and efficiency. The model’s central features are clearly defined roles for each team member, joint leader training, unit-level dashboards, and strong executive support. The result, the hospital exceeded its 2016 throughput target by 1,803 days, freeing 17 total beds while dramatically improving five key clinical measures.
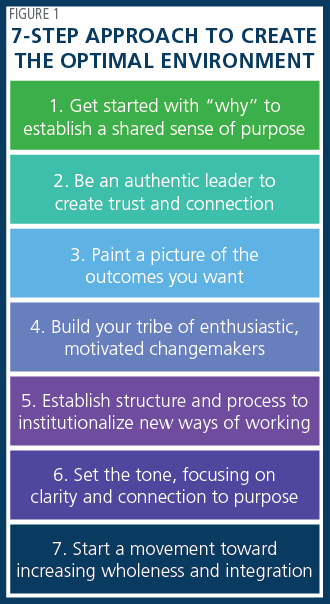 Dr. Michelle Janney, Executive Vice President and Chief Nursing Executive, and Dr. Jonathan Gottlieb, Executive Vice President and Chief Medical Officer, both of Indiana University Health (IUH), echoed the interprofessional theme in “Beyond Silos: Leveraging Systemness to Improve Quality.” They focused on a team process that reduced hospital acquired infections by 26%. Like North Shore, IUH combined nurse/physician leaders, interprofessional collaboration and accountability, a metrics dashboard, and a culture of transparency. Dr. Janney teamed with Andrea Kessler, IUH’s Vice President of Clinical Strategy and Integration, for a second presentation that emphasized the leader’s role in motivating diverse teams to pursue common purpose. In “Economies of Purpose: Maximizing Systemness for Impact,” Dr. Janney and Kessler offered a 7-step approach to create the optimal environment. (See Figure 1.)
Dr. Michelle Janney, Executive Vice President and Chief Nursing Executive, and Dr. Jonathan Gottlieb, Executive Vice President and Chief Medical Officer, both of Indiana University Health (IUH), echoed the interprofessional theme in “Beyond Silos: Leveraging Systemness to Improve Quality.” They focused on a team process that reduced hospital acquired infections by 26%. Like North Shore, IUH combined nurse/physician leaders, interprofessional collaboration and accountability, a metrics dashboard, and a culture of transparency. Dr. Janney teamed with Andrea Kessler, IUH’s Vice President of Clinical Strategy and Integration, for a second presentation that emphasized the leader’s role in motivating diverse teams to pursue common purpose. In “Economies of Purpose: Maximizing Systemness for Impact,” Dr. Janney and Kessler offered a 7-step approach to create the optimal environment. (See Figure 1.)
Strategies for Building Stronger Nursing and Leadership Pipelines
Growing demand for clinical leaders and staff combined with an increase in retirements and elevated turnover are driving and expanding the industry’s nursing shortages. To effectively respond, health systems and hospitals must build strong pipelines from entry level to senior nurse leadership. In “Establishing a Fully Oriented Staff Pipeline for Vacated Positions,” Yale New Haven Hospital’s Ena Williams, Interim Chief Nursing Officer, and Bette Ann White-McCullum, Nurse Manager, shared their organization’s approach to generating a candidate reserve by over-hiring and conducting orientation in advance of anticipated vacancies. The strategy reduces “premium spend dollars” often incurred when vacancies arise. Key to implementation was a transition from unit-based to service line-based hiring, supported by rigorous up-front analysis of personnel and financial data. Piloting a “cohort recruiting model” with an average 24 recruits per group, Yale New Haven has reduced turnover, increased available FTEs, and realized significant cost savings.
Derrick Garletts and Deanna Reising, both instructors at Indiana University, used the session “Developing Nurse Leaders: Collaboration Targeting the Quadruple Aim” to urge starting early in developing a leadership cadre. The two advocated partnerships between hospitals and health science programs to produce graduates with better leadership skills. In one example, teams of nursing and medical students underwent training and then conducted home visits to provide care to patients at high risk for hospital readmission. Faculty supervised via mobile video technology. The program yielded a dramatic drop in readmissions from 61% to 31%. Equally important, the students gained important clinical and interprofessional collaborative experience increasingly required for today’s clinical leaders.
The session “Using Emotional Intelligence to Build a Leadership Pipeline” placed the spotlight on an organization’s senior staff. The session was led by Julie Firman, Vice President and System Chief Nursing Officer at Southern Illinois Healthcare, and Innovative Connections Inc.’s Pat Samples, Vice President of Clinical Strategy and Operations, and Laurie Cure, Chief Executive Officer. Southern Illinois implemented a specific leadership coaching program to enhance Emotional Intelligence among leaders. The “Conscious Leader Program” expand the organization’s pipeline and developed existing leaders. Emotional Intelligence fosters a leadership mindset characterized by asking questions, listening, empowering team members to develop solutions, and collaboration. The speakers conveyed strong program results, including statistically significant higher Emotional Intelligence scores and a 15% promotion rate for participants, demonstrating a stronger internal leader pipeline.
Managing the Growing Millennial Workforce
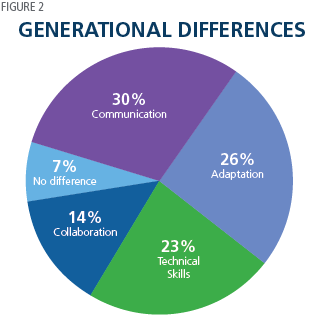
Millennials will account for 50% of the U.S. workforce by 2020 and 75% by 2030. Effectively managing this increasing group is or will be a priority for every clinical executive. In “Using Situational Leadership to Manage Multigenerational Employee Groups,” Jane Hokanson Hawks, Professor and Core Coordinator at Nebraska Methodist College, and Dr. Kathryn Spiegel, Adjunct Professor at Kaplan University School of Nursing, summarized a study ranking the dimensions on which the five workforce generations display the greatest differences, shown in Figure 2.
 The professors applied Hersey and Blanchard’s “theory of situational leadership” to formulate specific management approaches for each generation. The theory defines a leader’s mix of task and relationship behavior guidance in context of each individual’s readiness level. For Millennials, the speakers recommended:
The professors applied Hersey and Blanchard’s “theory of situational leadership” to formulate specific management approaches for each generation. The theory defines a leader’s mix of task and relationship behavior guidance in context of each individual’s readiness level. For Millennials, the speakers recommended:
- Communicate frequently
- Give consistent feedback
- Provide meaningful work activities
- Adopt a coaching style of management (versus top-down authoritative)
- Pair Millennials with mentors
- Offer work-life balance
The session “Connecting with Millennials to Understand the ‘Why’,” underscored the need for communication, coaching, and meaning. Texas Health Resources’ Joan Shinkus Clark, Senior Vice President and System Chief Nurse Executive, and Barbara Zepeda, Senior Specialist of Clinical Engagement and Nursing Communications, highlighted four best practices for communicating with Millennials:
- Address the “why”
- Ask for input
- Be transparent and personal
- Keep it brief and entertaining
The organization applied these principles creatively through a series of informal videos titled “Conversations with Joan.” The videos featured Millennial nurses talking with Clark. These pieces conveyed information, dug into the purpose behind the topics, and sought feedback on important issues such as “What do you think has been the greatest barrier to submitting information on adverse safety events?” The videos have been successful, averaging 770 views and 245 completed surveys per video, with 92% of respondents rating them “effective” or “very effective”.
Continuously Improving Nurse Education is a Leadership Priority
The National Education Progression in Nursing (NEPIN) is a collaborative working to improve academic nurse education. In “Power in Partnerships: Building the BSN Workforce,” Tina Lear, National Program Director for the National Education of Progression in Nursing Collaborative (NEPIN), was joined by Donna Meyer, Chief Executive Officer at the Organization for Associate Degree Nursing, Judith Berg, Chief Executive Officer at HealthImpact, and Jan Jones-Schenk, Academic Vice President of the College of Health Professions at Western Governor’s University. The group discussed the innovations needed to improve the workforce and encourage more nurses to achieve higher degrees. Addressing clinical education, accreditation, hiring practices and more, the panel proposed four priorities for change:
- Quality: Nationally accredited nursing education programs
- Cost: Affordability, ability to repay debt, and continue academic progression
- Access: Multiple learning options including online programs
- Impact on providers: Flexibility of schools to schedule clinical work with staff
Another training innovation involves the utilization of apprenticeships, a subject explored in the session “Funding Onboarding of New Nurses through Workforce Apprenticeships.” Yale New Haven Hospital’s Mary Cleary, Manager of Core Nursing Education, and Judith Hahn, Director of Professional Practice, explained how their organization aligned its onboarding process with the requirements of the U.S. Department of Labor apprenticeship program. Yale New Haven annually onboards 400 nurses. Aligning with the apprenticeship program enabled the hospital to fund “a business-driven model that combines on-the-job training with related technical instruction” in which apprentices “earn and learn.” The government has allocated $90 million to support such trade apprenticeships. The apprenticeships have generated positive reception from first year nurses.
Aligning nurse training with organizational strategy and realizing a return on the investment are becoming imperatives. It was the focus of the session, “Results Oriented Education: Innovation in Assessment and Delivery Methods Based on Learner Style Preference,” by Bridget Tippins, Manager of Clinical and Patient Education, and Noel Arring, Manager of Nursing Research, at the Mayo Clinic. Four barriers frequently compromise effectiveness:
- Often same practice issues repeated
- Education priorities set in response to specific issues
- Everyone receives same education
- Strategic alignment lacking
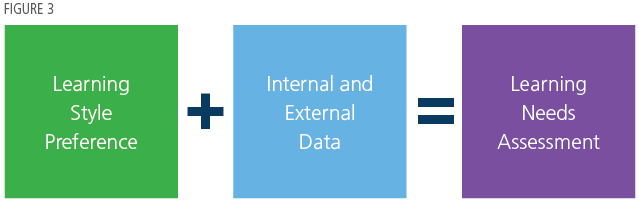 Learner-centered education is crucial or success. Strategic priorities should guide education topics, and learning assessments must be individually tailored and data-driven, as summarized in Figure 3. The session concluded with the recommendation that ROI for nurse education is best measured by improved patient outcomes.
Learner-centered education is crucial or success. Strategic priorities should guide education topics, and learning assessments must be individually tailored and data-driven, as summarized in Figure 3. The session concluded with the recommendation that ROI for nurse education is best measured by improved patient outcomes.
Technology Driving Productivity and Patient Care
 Several presentations showcased innovative uses of technology to improve both efficiency and patient outcomes. For example, in “Modernizing Clinical Communications for the Mobile Workforce,” Rosemary Ventura, Chief Nursing Informatics Officer, and Leo Bodden, Vice President and Chief Transition Officer, at New York-Presbyterian Hospital (NYP) described deployment of a unified mobile platform for 17,000 caregivers across 10 facilities. The goal was to replace a fragmented, multi-device, separate app environment, with an integrated solution providing access to phone, texts, broadcast messages, contacts, and patient information accessible from one screen. (See Figure 4.)
Several presentations showcased innovative uses of technology to improve both efficiency and patient outcomes. For example, in “Modernizing Clinical Communications for the Mobile Workforce,” Rosemary Ventura, Chief Nursing Informatics Officer, and Leo Bodden, Vice President and Chief Transition Officer, at New York-Presbyterian Hospital (NYP) described deployment of a unified mobile platform for 17,000 caregivers across 10 facilities. The goal was to replace a fragmented, multi-device, separate app environment, with an integrated solution providing access to phone, texts, broadcast messages, contacts, and patient information accessible from one screen. (See Figure 4.)
The solution has greatly improved communication and is now further aiding care by delivering mobile, AI-enhanced clinical decision support.
The session “Huddled-Up and Wired to a Real-Time Electronic Dashboard,” demonstrated the substantial benefits accruing to data analytics technology. Lehigh Valley Health’s Marie Kim Jordan, Chief Nursing Officer, and Dr. David Burmeister, Chair of Emergency Medicine, explained how their organization utilized its electronic health record to improve clinical care. The hospital’s management had been huddling daily to address increased lengths of stay, ambulance diversions to other hospitals, as well as admissions for patients languishing in the ED. A breakthrough occurred with the development of an EHR-based automated dashboard, organized around workflow and key metrics. The dashboard reduced manual preparation, synthesized information, and provided real-time data needed to drive decisions. Results included decreased length of stay by 5% (translating into 34,200 additional bed hours), zero ED diversions with no patient turned away, and 1,500 more admissions than budgeted.
Conclusion
The AONE 2018 conference offered vigorous discussion of important issues in management, leadership development, and technology. More important, nurse leaders gained valuable advice and best practices on these subjects which they can put into practice immediately.
Read More