B.E. Smith Team | November 25, 2018
Executive Brief: Four Strategic Topics in Focus at Becker’s CEO & CFO Roundtable
Becker’s Hospital Review CEO and CFO Roundtable continues to be a highly illuminating conference. The just-concluded forum was no exception, with fresh insights delivered on strategic issues. B.E. Smith actively participated and highlights four themes that garnered significant attention.
Many Opportunities to Advance Value-Based Care
Top executives remain focused on meeting the demands of new value-based care reimbursement models (VBC). Several CEOs canvassed this subject. In “Challenges and Opportunities: The Future of Value-Based Care,” Jeffrey Hulburt, CEO at Beth Israel Deaconess, proposed three guiding approaches:
- Set realistic performance targets in risk contracts. Payer-provider collaboration is essential here to “honestly and accurately assess each party’s strengths and contributions.”
- Unify standards of care. Organizations can adhere to “shared principles of primary care” such as the eight promulgated by the Patient Centered Primary Care Collaborative.
- Understand the role and influence of politics. Government regulations have been consistently cited in B.E. Smith surveys as the top change driver. Hulburt urged CEOs to get educated on the political environment affecting VBC, “have a seat at the table at local and federal levels,” and voice opinions.
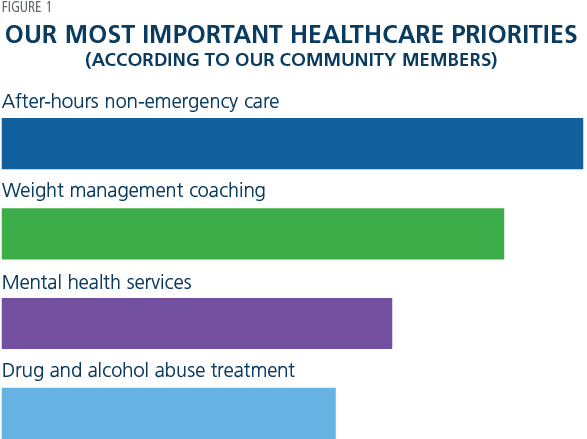 Small and rural hospitals face particular challenges in achieving value-based care. That was the theme of “Tools for Implementing Value-Based Care Initiatives in Rural/Frontier Healthcare Delivery Systems,” by Benjamin Anderson, CEO, Kearny County Hospital, and Jordan Millhollin, a Baylor University student. In a series of entertaining statements, the speakers challenged common thinking, such as “we know our patients by name and provide access to great care.” The responses were that “knowing your patients’ names does not equal great outcomes” and “how can you prove you provide great care?” They then detailed how Kearny used a rigorous door-to-door community wellness survey to develop strategies. The top four priorities, displayed in Figure 1, are shared by many rural communities.
Small and rural hospitals face particular challenges in achieving value-based care. That was the theme of “Tools for Implementing Value-Based Care Initiatives in Rural/Frontier Healthcare Delivery Systems,” by Benjamin Anderson, CEO, Kearny County Hospital, and Jordan Millhollin, a Baylor University student. In a series of entertaining statements, the speakers challenged common thinking, such as “we know our patients by name and provide access to great care.” The responses were that “knowing your patients’ names does not equal great outcomes” and “how can you prove you provide great care?” They then detailed how Kearny used a rigorous door-to-door community wellness survey to develop strategies. The top four priorities, displayed in Figure 1, are shared by many rural communities.
Kearny decided all solutions required improved health equity. Four “practical steps” were recommended:
- Determine the facts about adequacy of primary care for all.
- Critique proposed models of healthcare delivery in disadvantaged communities by asking whether we would settle for them if they were options being planned for us.
- Insist on a timeline for improved population-level outcomes.
- Examine availability of services from government, faith community, and other social organizations in areas with high unemployment.
The final advice was to “address macro problems with micro solutions:”
- If necessary, find temporary funding for the right things.
- Measure outcomes and cost related to each intervention.
- Share success with the people who hold the purse strings.
James Doulgeris, CEO, Osler Health, offered his organization’s VBC experiences, starting with such challenges as disparate EHR platforms and communication/care gaps. Osler’s solution portrays the need to effect “systemic changes” (Figure 2).

To change behavior “value-based care style,” Osler instituted full-screen interactive video as one tool for patient reminders and education. The upshot: high measured patient engagement and ability to create personalized experiences.
Build a High-Performance Organization
The value-based environment increasingly rewards the high-performance organization. Various performance improvement methods were presented. In “Change Leadership: How to Improve Your Hospital’s Bottom Line, Performance Metrics, and More,” Lynn Torossian, CEO, Henry Ford West Bloomfield Hospital, emphasized the need to drive financial and operational change. She posed four questions as a blueprint:
- What if you create an appetite for experimentation?
- What if you make change safer than the status quo?
- What if every leader in your organization made eight changes every month?
- What if leaders created CFO-validated savings, understood and managed productivity and engaged their teams?
Henry Ford’s answers were evidenced by many positive changes such as an 8.6% decrease in costly inpatient discharges in one year. Torossian concluded with a vigorous call to “continuously develop all leaders” as change agents.
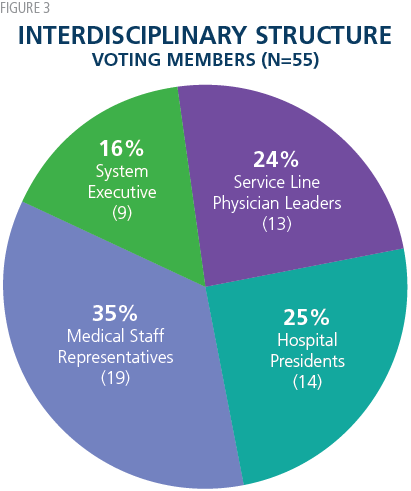
Howard Kern, CEO of Sentara Healthcare, shared his organization’s experiences in “Executing a System Strategy for Top Performance.” Several years ago, Sentara found itself falling behind its peers and struggling with organizational silos and too many initiatives. A systems approach was developed, founded on a high-performance structure involving:
- An interdisciplinary Clinical Leadership Council (Figure 3 shows the well-balanced composition).
- Interdisciplinary Horizontal Teams of management, physician, nurse, and ancillary leaders.
- Oversight by traditional vertical senior management: CEO, CFO, CMO.
 Sentara’s changes resulted in meaningful longrun performance improvements across the system in such critical areas as impatient mortality, ALOS, and HCAHPS scores. Kern offered five keys to success:
Sentara’s changes resulted in meaningful longrun performance improvements across the system in such critical areas as impatient mortality, ALOS, and HCAHPS scores. Kern offered five keys to success:
- Focus on reducing unnecessary clinical variation.
- Monitor actively to sustain gains.
- Prioritize opportunities and execute with interdisciplinary teams.
- Reinforce a performance improvement culture.
- Become “a highly predictable organization.”
In “Time Matters … the New Strategic Imperative,” Michael Sachs, Chairman of Repp Health, examined the nexus between better performance and care process analysis. The “patient work process can be measured and standardized.” For example, analytics revealed that Repp’s surgery patients admitted on Wednesdays “stayed an extra day for no reason.” Reducing steps and wait times directly saved money via reduced staffing, better capacity utilization and retention from higher patient satisfaction. Two key takeaways:
- Create a culture of “Time Matters.”
- Accelerate the pace of care by analyzing data and real-time patient movement.
Choose Optimal Financial Strategies
Today’s organizations confront strategic choices carrying significant financial implications. Lee Domanico, CEO, Marin General Hospital, used “Beating the Odds as a Free-Standing Hospital in a Highly Competitive Metropolitan Area” to address whether a community hospital can or should remain independent. Part of a public system, Marin’s challenges included quality concerns, need for a new facility and net cash outflows to the parent organization. The hospital’s choice to become independent entailed considerable financial drama. The early years saw declining volume and receivables write-downs contributing to a $40 million cash flow drain. The organization was able to tap credit markets and philanthropy to build the new hospital. Though stabilized, Marin knew it needed network alliances to survive and found the right partner in UCSF. A mutually beneficial arrangement included a capital infusion and access to UCSF’s EHR. Domenico offered the relevant considerations about independence, shown in Figure 4.

His concluding advice:
- Don’t give away your hospital.
- Consider other options to merger or sale.
- Act while you are strong financially.
B.E. Smith’s Executive VP Mike Supple moderated a panel examining the opposite perspective: how to build a successful integrated health system. Trevor Wright, COO, Loma Linda University Health, Kate Henderson, regional president, Seton Medical Center, and David Clark, executive with large system experience, exchanged ideas in “Health System Consolidation and Integration: Optimization of the Operating Company Model.” Three major drivers for the model were cited:
- Cost savings from reduced variability in care delivery and operations.
- Ability to market a new brand promise of providing a common care experience throughout the system.
- Management flexibility in moving talent across and within the system entities.
Among the panel’s many takeaways, three were emphasized. First, consistently communicate consolidation’s rationale and advantages. Wright suggested, “What resonates isn’t just talking about reduced costs but about being a better healthcare delivery entity.” Henderson concurred, “Consolidation frequently generates a sense of loss, so … it’s required of leaders to make sure we are messaging the opportunity” and engaging the community. The panel also counseled assessing organizational readiness to integrate. Clark observed that many institutions are not ready for consolidation, some because “it is really tough when things are going well to make changes.” Finally, an “agile” rather than a “Big Bang” rollout of the operating structure can prevent disruption and encourage helpful change iterations over time.
A different financial strategy many have considered was covered by Susan Hawkins, Senior VP at Henry Ford Health System (HFHS), in “Lessons for Contracting Directly with Employers.” She detailed the decision to enter with General Motors a “five year Direct-to-Employer value-based contract.” A core feature is risk sharing, with incentives based on public quality metrics. GM expects lower total cost of employee health with improved wellness, while HFHS sees volume growth through increased market share and “keepage” of existing GM patients. The presentation closed with pragmatic guidance:
For health systems
- Create a multidisciplinary team to be on “the other side of the RFP process.”
- Assess network adequacy up front.
- Be prepared to accept contract carve-outs for areas such as pharmacy and behavioral health.
- Communicate extensively with executives, physicians, and partners.
For employers
- Conduct a formal contract process with clear goals.
- Gather and share extensive data on employees.
- Recognize that employees generally have limited understanding of healthcare and benefits.
Security Threats Demand Continued Vigilance
Technology remains top of mind for healthcare’s C-suite. One universal technology concern was explored in “HIT Security, Ransomware, and Enterprise Risk Management” by Mitchell Parker, CISO at Indiana University Health. His wide-ranging presentation on effective cybersecurity spotlighted several strategies:
- Avoid custom software. Maintenance is difficult, the “risk of infection goes up significantly,” and “a high degree of customization means that fixes for security often have issues.”
- Move away from legacy systems. They are highly vulnerable to attack, and “recovering from one will be expensive if not impossible.”
- Create a formal risk scoring system. Assess enterprise risk using consistent metrics and ensure that everyone monitors the status.
- Dedicate a team to execute threat assessment and set standards for the organization.
Conclusion
Conference attendees learned about real progress and continuing challenges in vital strategic areas such as delivering value-based care, improving organizational performance, pursuing transformational financial strategies and attending to cybersecurity threats. Takeaways were numerous, ready to implement, and valuable.
Read More